Can Diabetic Retinopathy Be Reversed? Exploring Treatment Options

Diabetic retinopathy is one of the four main eye conditions linked to diabetes and is a leading cause of blindness in adults worldwide. It can affect individuals with type 1, type 2, and gestational diabetes and occurs when high blood sugar levels damage the tiny blood vessels in the retina, leading to vision impairment.
Generally, damage from diabetic retinopathy is not reversible. However, treatments can help slow or stop the progression of the disease. Here’s how diabetic retinopathy is diagnosed and treated, as well as key prevention tips.
The Four Stages of Diabetic Retinopathy
There are two main types of diabetic retinopathy: non-proliferative (NPDR), which is the most common type, and proliferative, the most advanced, severe type. The condition progresses through four stages:
- Mild NPDR: Small blood vessels in the retina begin to swell in this earliest stage. These areas of swelling are known as microaneurysms and are a significant indication of worsening diabetic retinopathy. These microaneurysms weaken the blood vessels, causing small amounts of fluid and blood to leak into the retina and the macula — the central part of the retina — to swell.
- Moderate NPDR: Swelling increases in this stage, and more blood vessels become blocked and damaged, leading to reduced blood supply to the retina and more fluids accumulating in the macula.
- Severe NPDR: Blood flow becomes significantly impaired in this stage as more blood vessels become blocked. The retina signals the body to grow new, abnormal blood vessels to help transfer oxygen.
- Proliferative retinopathy: The new blood vessels form, but their frailty elevates the risk of fluid leakage into the vitreous humor, the clear gel-like substance that fills the space between the eye’s lens and retina. The vessels can bleed, scar, and cause severe vision problems, including retinal detachment.
Diagnosing Diabetic Retinopathy
The risk for diabetic retinopathy increases the longer you have diabetes, especially if glucose levels remain unmanaged. Symptoms often aren’t noticeable during the early stages. Still, individuals may experience subtle changes in vision that may come and go, such as difficulty reading or seeing objects at a distance. In later stages, symptoms may become more pronounced and include:
- Blurry vision
- Floaters
- Faded colors
- Blank or dark areas in the field of vision
Early diagnosis of diabetic retinopathy is critical to prevent irreversible vision loss and supports better treatment outcomes. Regular comprehensive dilated eye exams and diabetic eye exams help your ophthalmologist detect diabetic retinopathy before symptoms become noticeable. These exams are very similar, with significant overlap in the tests performed, but diabetic eye exams focus more specifically on the retina to monitor and detect diabetes-related eye complications. During these exams, your eye doctor may:
- Ask about your family history.
- Perform a visual acuity test
- Measure your eye movement
- Determine refractive error and prescription
- Examine your eyes with a slit lamp
- Administer special drops to dilate or widen your pupils for a closer look at the lens, retina, and optic nerve.
Your ophthalmologist can also check for other potential eye conditions that can be caused by diabetes, such as glaucoma or cataracts. Retinal imaging, including color fundus photography, optical coherence tomography (OCT), or fluorescein angiography, reveals swelling, fluid leakage, and circulation concerns of the blood vessels and retina.
Preventing and Treating Diabetic Retinopathy
You can help prevent diabetic retinopathy by actively managing your diabetes. Practicing these key steps can help keep your blood sugar, blood pressure, and cholesterol in healthy ranges:
- Regularly monitoring your blood sugar
- Prioritizing physical activity
- Eating a nutritious diet
- Taking all insulin and other diabetes medications as prescribed
Although vision loss from diabetic retinopathy is irreversible, treatments can slow or halt its progression and prevent further damage. The potential for improvement depends on how advanced the condition is. Treatments include:
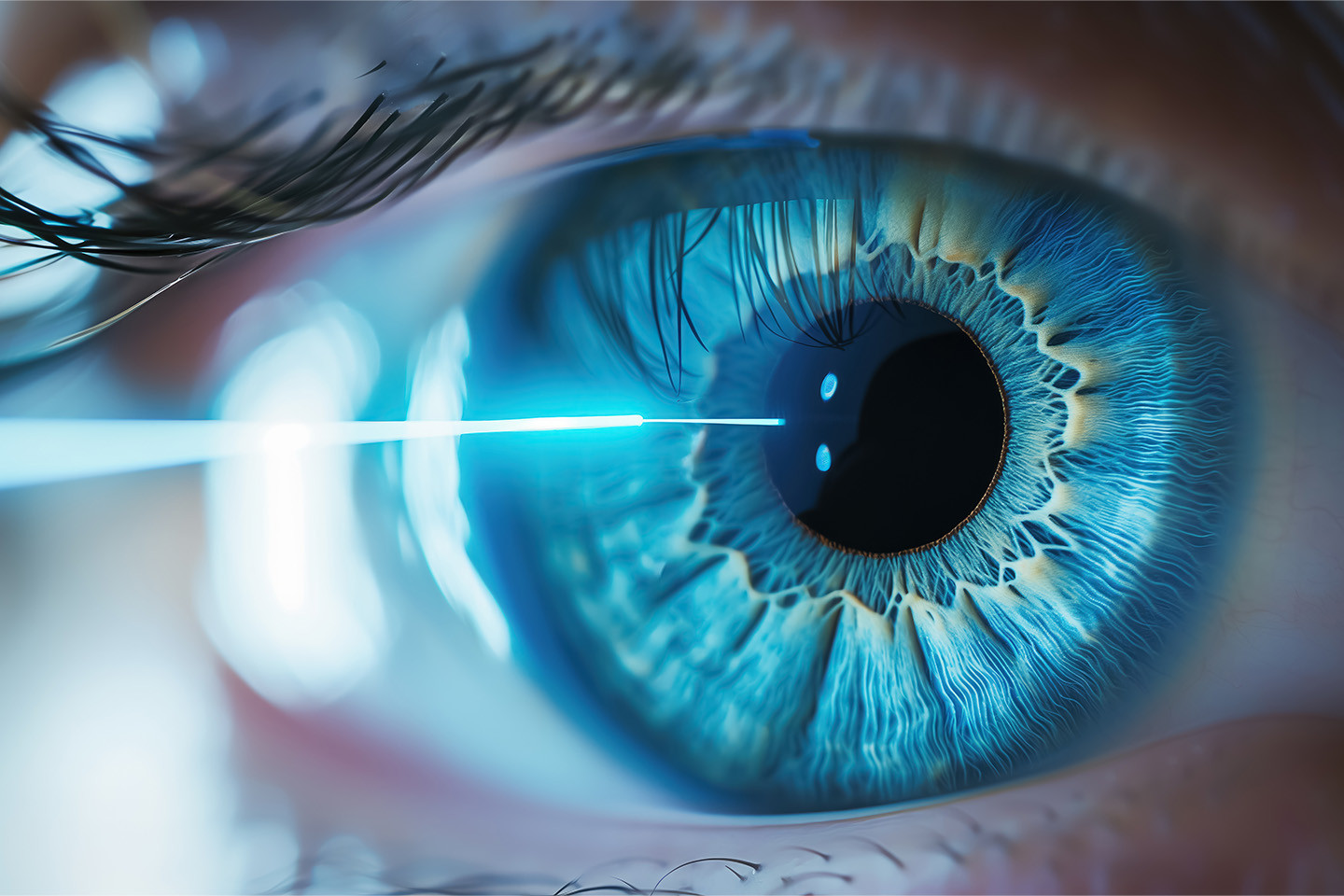
- Laser treatment: Photocoagulation (focal laser treatment) and panretinal photocoagulation (PRP, or scatter laser surgery) are both forms of laser treatment typically performed in a doctor’s office or eye clinic. Photocoagulation seals leaking blood vessels and helps reduce swelling in the retina, while PRP is used to shrink abnormal blood vessels and prevent further growth.
- Anti-VEGF therapy: In cases of proliferative diabetic retinopathy, abnormal blood vessel growth is driven by a protein called vascular endothelial growth factor (VEGF). Anti-VEGF injections block this protein, preventing the growth of these blood vessels. These injections are administered directly into the eye and are highly effective in reducing fluid buildup in the retina, stabilizing vision, and, in some cases, improving it.
Treatment usually begins with monthly injections and continues as needed. In some cases, anti-VEGF therapy is combined with photocoagulation.
- Corticosteroid injections: Corticosteroid injections into the eye can help reduce inflammation and swelling in the retina. This treatment is often used in combination with anti-VEGF therapy, especially in cases of diabetic macular edema (DME), a common complication of diabetic retinopathy.
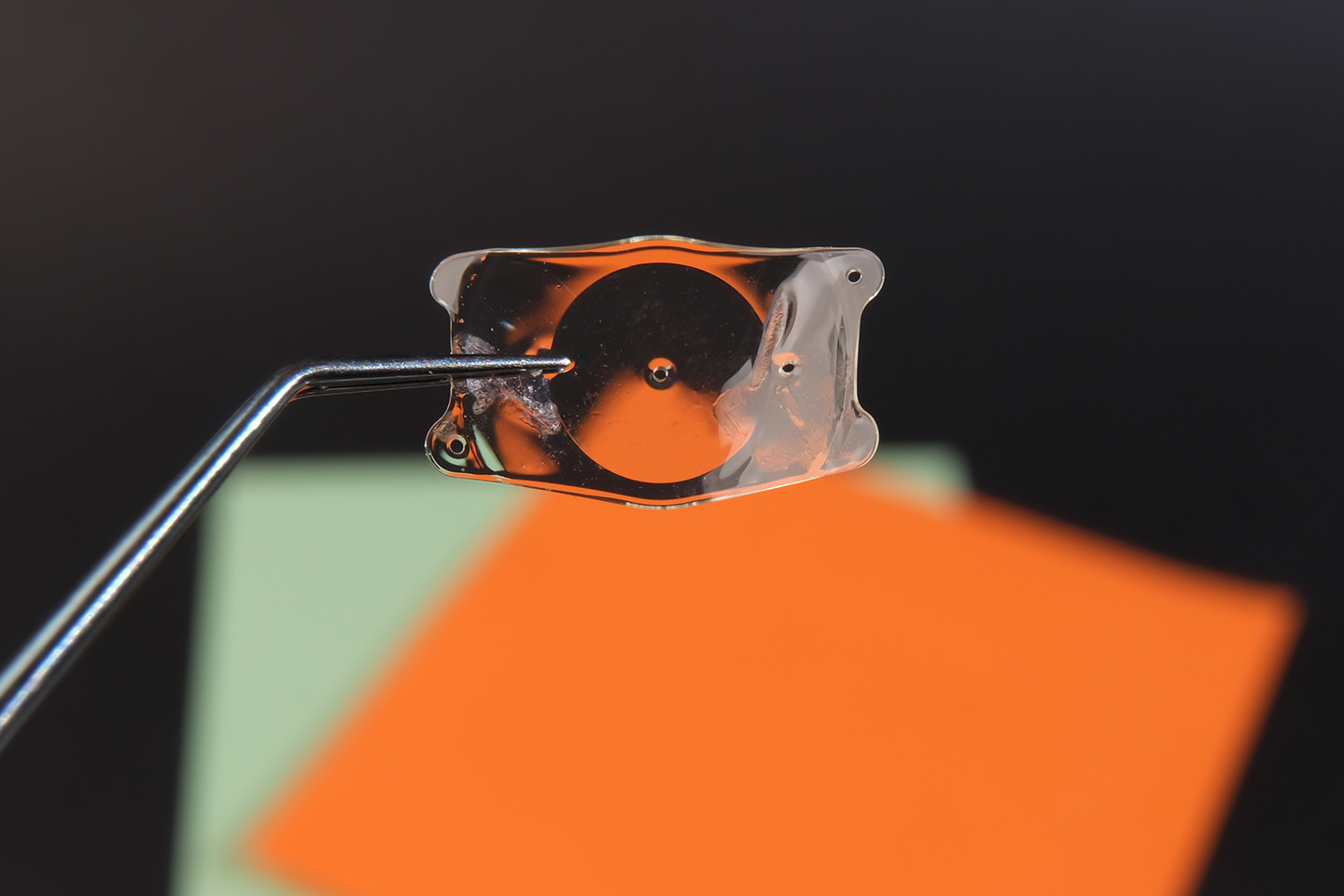
- Vitrectomy: A vitrectomy may be necessary for advanced cases of diabetic retinopathy involving bleeding into the vitreous or when retinal detachment is a concern. The procedure involves making a small incision to remove the vitreous gel and any blood or scar tissue. The surgeon may also repair or reattach the retina as needed or inject an air bubble, other gas, or silicone oil into your eye to hold your retina in place.
- Vitrectomies are typically performed one eye at a time in a hospital or surgery center, using local or general anesthesia. Most people go home the same day. Recovery can take several weeks; depending on the treatment plan, you may require a second procedure. Eventually, the eye will naturally replace the removed vitreous with new fluid.
Your Local Eye Care Experts
Regular comprehensive eye exams are important for everyone, but it’s especially crucial for individuals with diabetes to follow recommended eye exam schedules and discuss any vision or eye health changes with their eye doctor. Contact ICON Eyecare today to learn about our advanced diagnostic testing and how we can help you achieve and maintain optimal vision.
[DISPLAY_ULTIMATE_SOCIAL_ICONS]