Does Diabetes Cause Cataracts?

Cataracts and diabetes are two prevalent health conditions that affect millions of people worldwide. But how do they relate to one another?
Diabetes is a chronic condition that affects how insulin helps the body process food into sugar (glucose) and convert it to energy. It can lead to and compound other health problems, including heart disease, kidney disease, and nerve damage. According to the Centers for Disease Control and Prevention (CDC), 38.4 million Americans — 11.6% of the population — had diabetes in 2021, and that number is projected to rise by 2030.
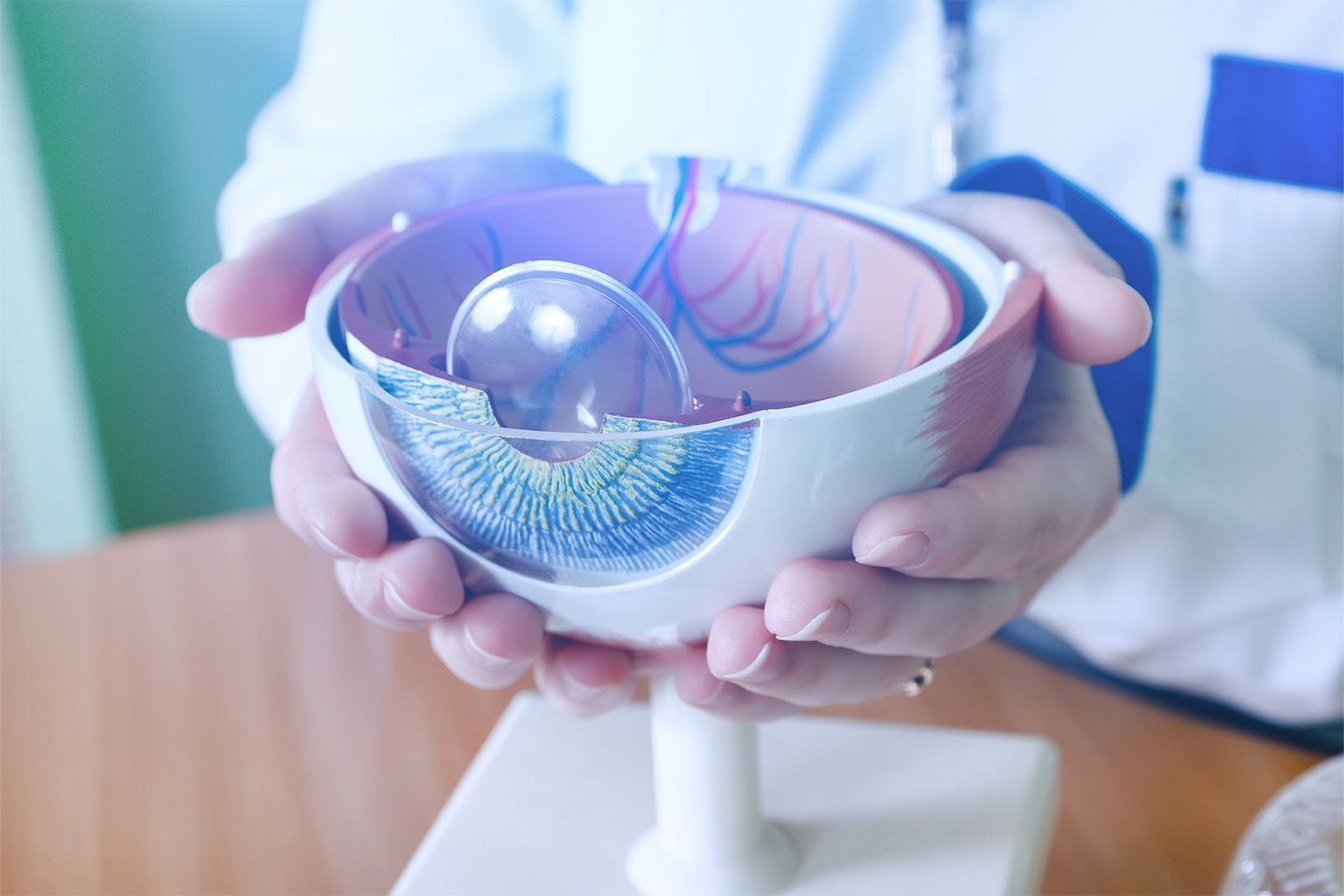
Cataracts cloud the eye’s natural lens and are one of the leading causes of vision loss and blindness globally. According to the National Eye Institute, more than half of all Americans age 80 or older have cataracts or have had cataract surgery. While cataracts are commonly associated with age-related vision changes, uncontrolled blood sugar can significantly increase the risk of cataract development.
The Impact of Diabetes on Vision Loss
Diabetes’s effect on the body can be complex and multi-faceted. In addition to cardiovascular and neurological health conditions, diabetes can also increase the risk of eye disease, such as diabetic retinopathy, macular edema, cataracts, and glaucoma. These conditions can lead to vision loss or blindness due to blood vessel damage, pressure, and other issues caused by high blood sugar. According to a 2019 data brief from the CDC, 32% of adults aged 45 and over with diabetes had cataracts, 8.6% had diabetic retinopathy, 7.1% had glaucoma, and 4.3% had macular degeneration.
How High Blood Sugar Affects Cataract Development
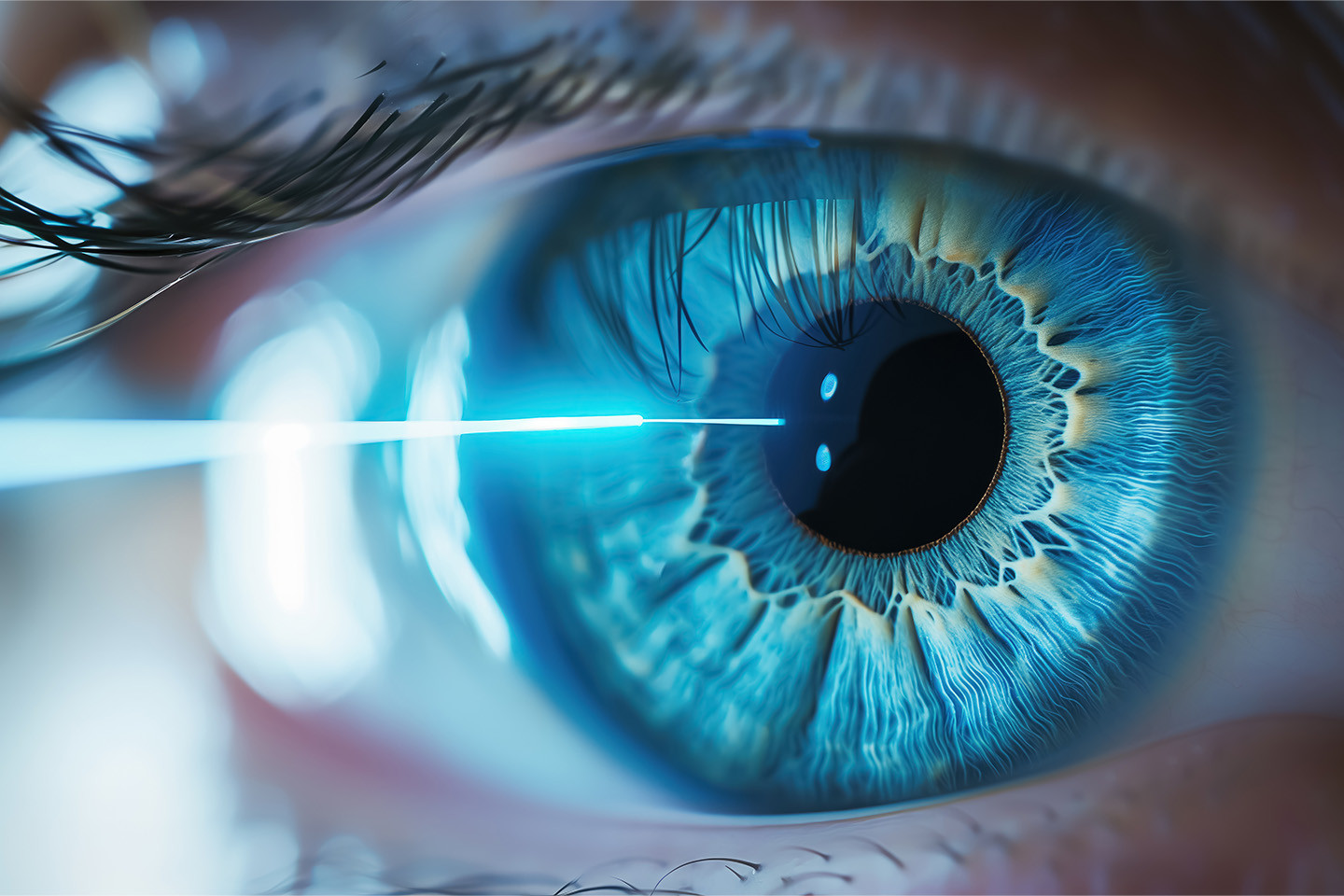
Cataract development is most often associated with age. Proteins called crystallins in the eye’s natural lens break down over time, causing the lens to become cloudy and vision blurred or hazy. This cloudiness is the cataract.
For individuals with diabetes, cataracts are often the result of high sugar levels in the aqueous humor. This clear fluid between the lens and cornea provides oxygen and glucose to the lens. When glucose isn’t regulated, the sugar levels in the aqueous humor increase, leading to elevated glucose levels in the lens and compromising vision.
Excess sorbitol in the lens is another factor in diabetic cataract development. Sorbitol is a sugar alcohol found naturally in many fruits and vegetables and is often used as an artificial sweetener. When blood sugar levels are high, enzymes in the lens may produce sorbitol to help process glucose. However, sorbitol can accumulate in the lens, causing osmotic stress that affects the lens’s structure and accelerates cataract formation.
Mitigating Your Risk of Cataract Development
Your risk of developing cataracts depends on how long you have been a diabetic patient, how frequently your blood sugar spikes above your target range, and if you have macular edema. Studies suggest that individuals with diabetes may be up to five times more likely to develop cataracts, particularly at an earlier age. With the continued rise of diabetes, the incidence of diabetic cataracts also continues to increase.
No one can truly prevent cataracts. However, individuals with diabetes can take steps to lower their risk. Maintaining healthy blood glucose levels by monitoring blood sugar and adhering to medication schedules, making healthy lifestyle adjustments (such as increasing physical activity or avoiding tobacco), and regular comprehensive eye exams are crucial to mitigating your risk of developing cataracts.
Cataract Surgery and Considerations for People with Diabetes
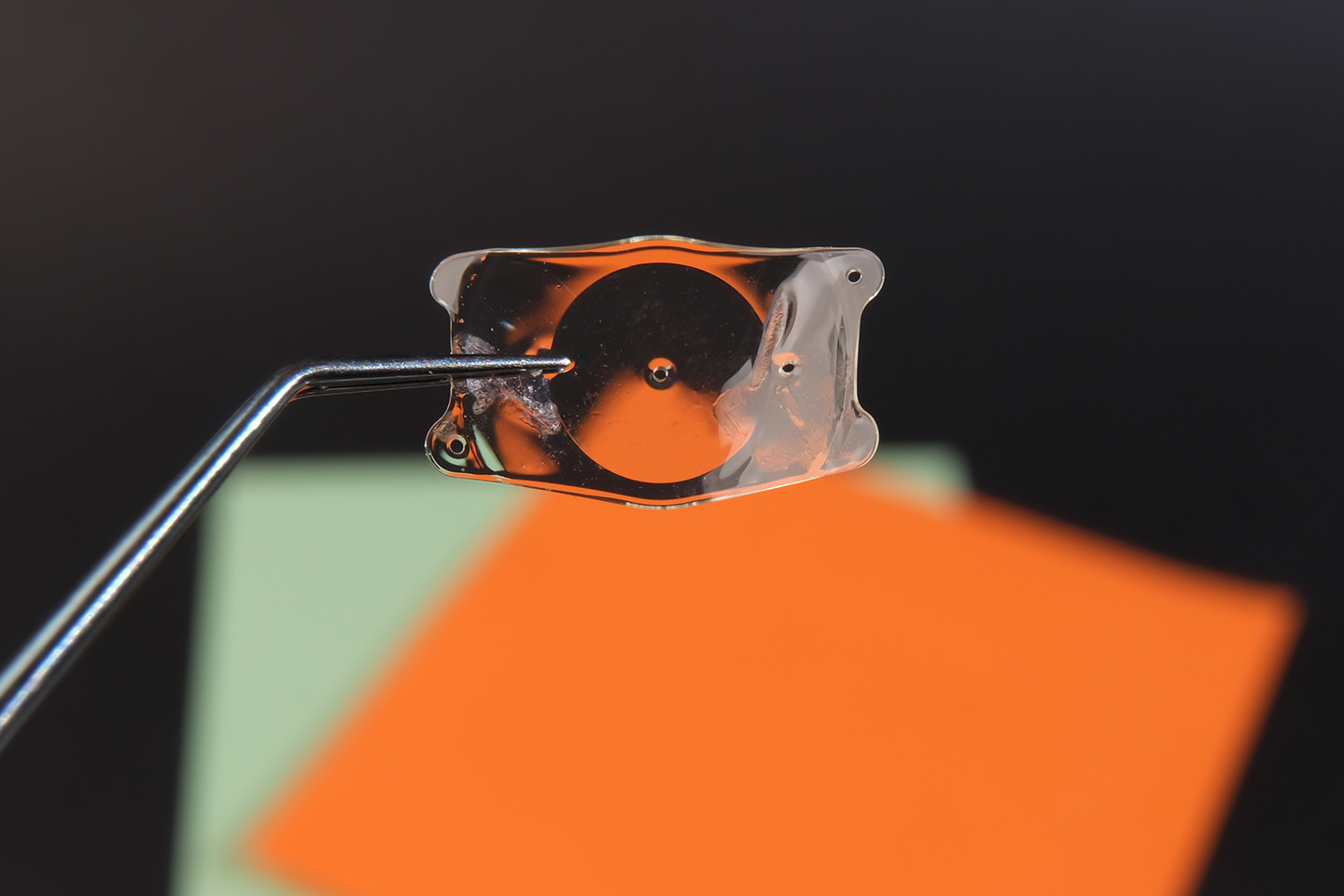
Cataract patients will eventually experience significant vision loss or blindness without treatment, but cataract surgery is a safe, effective, and proven way of restoring vision. During this quick procedure, an eye surgeon removes the damaged lens and replaces it with a clear intraocular lens (IOL).
Individuals with diabetes should take special consideration to ensure successful outcomes from cataract surgery:
- Maintain optimal blood sugar control. High blood sugar can affect post-surgery healing and increase the risk of infection or bleeding.
- Undergo a preoperative diabetic eye exam. Understanding your overall eye health is vital to identifying and treating other preexisting conditions that may lead to complications, including diabetic retinopathy or macular edema, which may require additional treatment or monitoring alongside cataract surgery.
- Research and select an experienced surgeon. It’s essential to choose a surgeon with experience and expertise in treating patients with diabetes-related eye conditions. A skilled surgeon will be familiar with the unique challenges diabetes presents and can tailor the surgical approach accordingly to minimize risks and optimize outcomes.
- Know the risks. As with all surgical procedures, cataract surgery is not without its risks. Individuals with diabetes may be prone to additional complications, including decreased sensitivity in the cornea, endophthalmitis (a rare but severe infection that presents more commonly in patients with diabetes compared to those without), increased swelling in the macula, and worsening of diabetic retinopathy.
- Understand IOL choices may be limited. Selecting an IOL that meets vision and budget goals is crucial for any cataract surgery. For individuals with diabetes, however, options may be limited depending on the presence of preexisting conditions that can impact visual outcomes after surgery, like diabetic macular edema or an irregular corneal surface. It’s important to discuss the most appropriate type of IOL, such as toric or multifocal lenses, based on your needs and eye health.
- Adhere to all pre- and post-operative instructions carefully. Eye surgeons commonly prescribe eye drops before cataract surgery to help prevent infection and promote better healing. These drops are especially important for patients with diabetes to reduce the risk of complications. Discuss all current medications with your eye surgeon; they may instruct you to avoid certain medicines on the day of your surgery. After your surgery, your eye surgeon may prescribe steroid and anti-inflammatory eye drops and schedule follow-up visits; using them as recommended and attending all post-operative appointments are vital to a healthy healing process.
Trust Colorado’s Cataract Experts at ICON Eyecare
At ICON Eyecare, we can help you navigate cataract surgery with confidence and safeguard your vision for years to come. Our expert team of world-class surgeons and eye doctors prioritizes your safety and the quality outcome you deserve. Contact us today if you’re experiencing signs of cataracts and are ready to take the first step to protect and restore your vision with our treatment options.
[DISPLAY_ULTIMATE_SOCIAL_ICONS]