Category: Eye Care

How LASIK at ICON Eyecare Front Range Helped Me Overcome Astigmatism

How Successful is Clear Lens Exchange? Expert Insights from an ICON Eyecare Ophthalmologist.

Can Diabetic Retinopathy Be Reversed? Exploring Treatment Options

How Diabetes Impacts Eye Health: Conditions and Prevention Tips

8 Tips To Prevent Your Glaucoma from Worsening
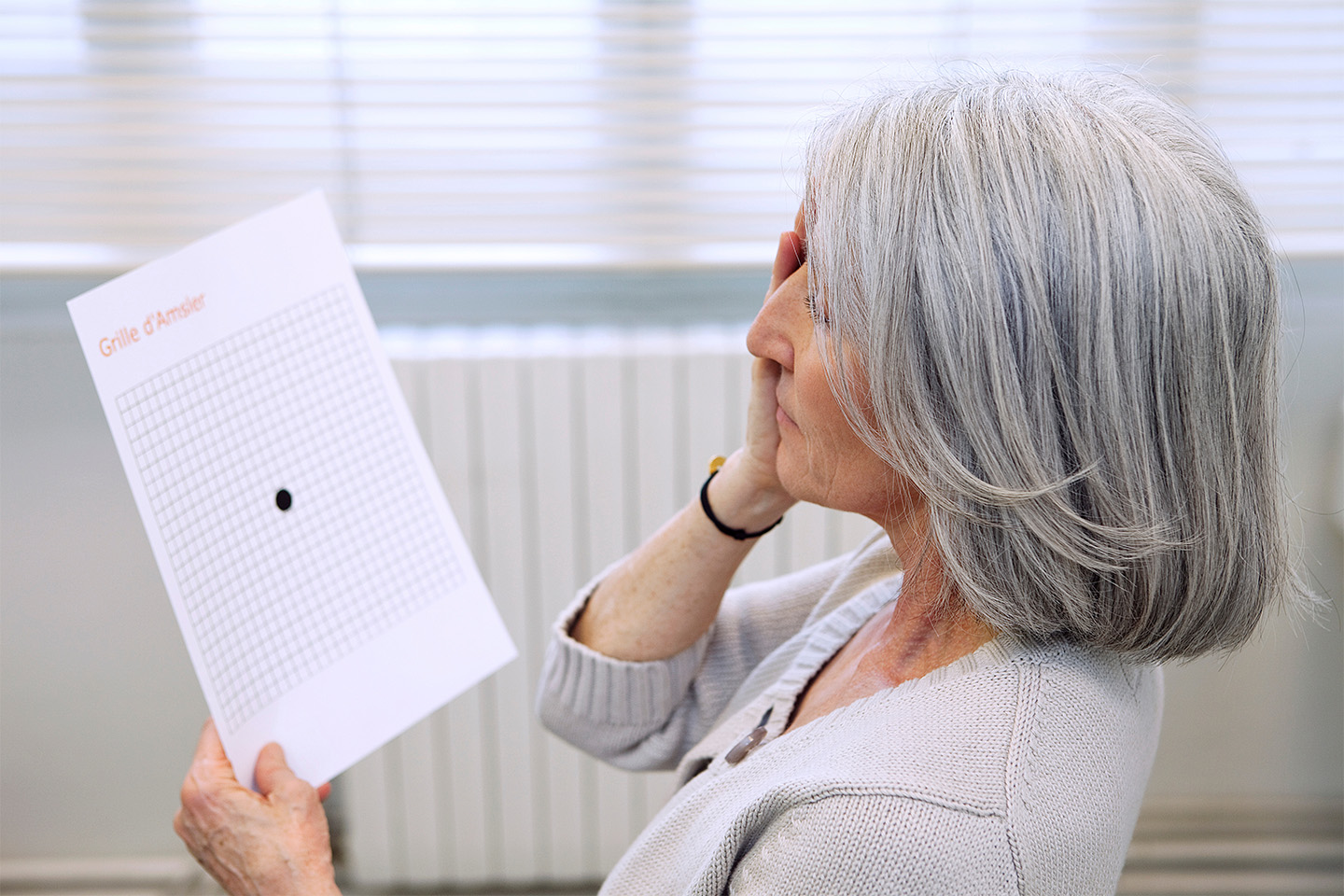
Monitoring Your Vision: How the Amsler Grid Vision Test Gives Insights Into Eye Health

Is Clear Lens Exchange Covered By Insurance?

What is a Diabetic Eye Exam?

How Long Should You Wait Between Cataract Surgery on Each Eye?

Can You Really Get Glaucoma in Your 20s?