Eye Care Series: Symptoms of Keratoconus

At ICON Eyecare, our leading ophthalmologists in the Front Range diagnose and treat many less-common eye conditions such as keratoconus. It’s one of the reasons that people prefer us for regular eyecare, eye exams, and services such as cataract and LASIK surgery in the Denver metro area. Our knowledge and experience help us give you the best outcomes to improve your vision and protect your eye health.
Vision Impairment from Distorted Cornea Shape in Keratoconus
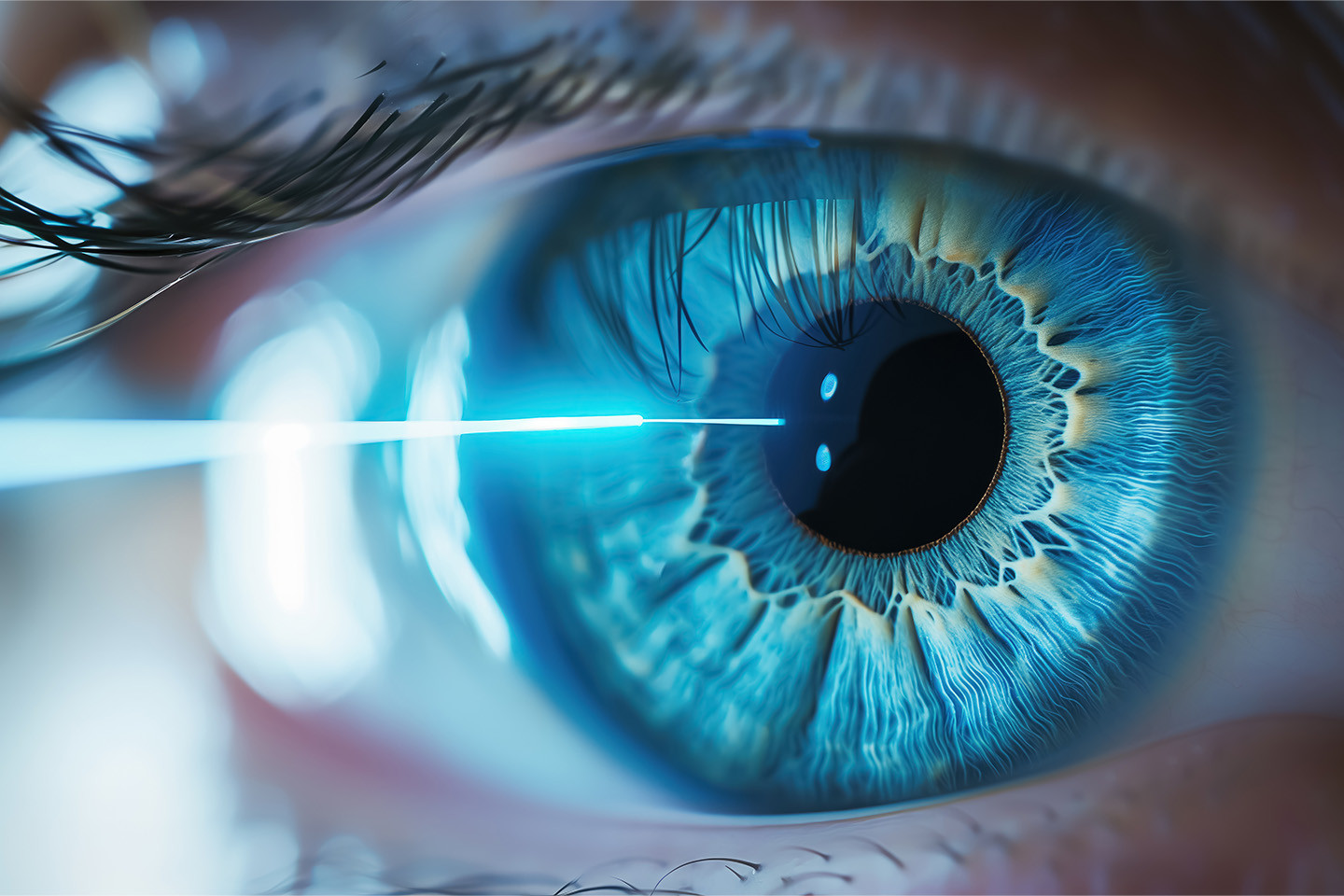
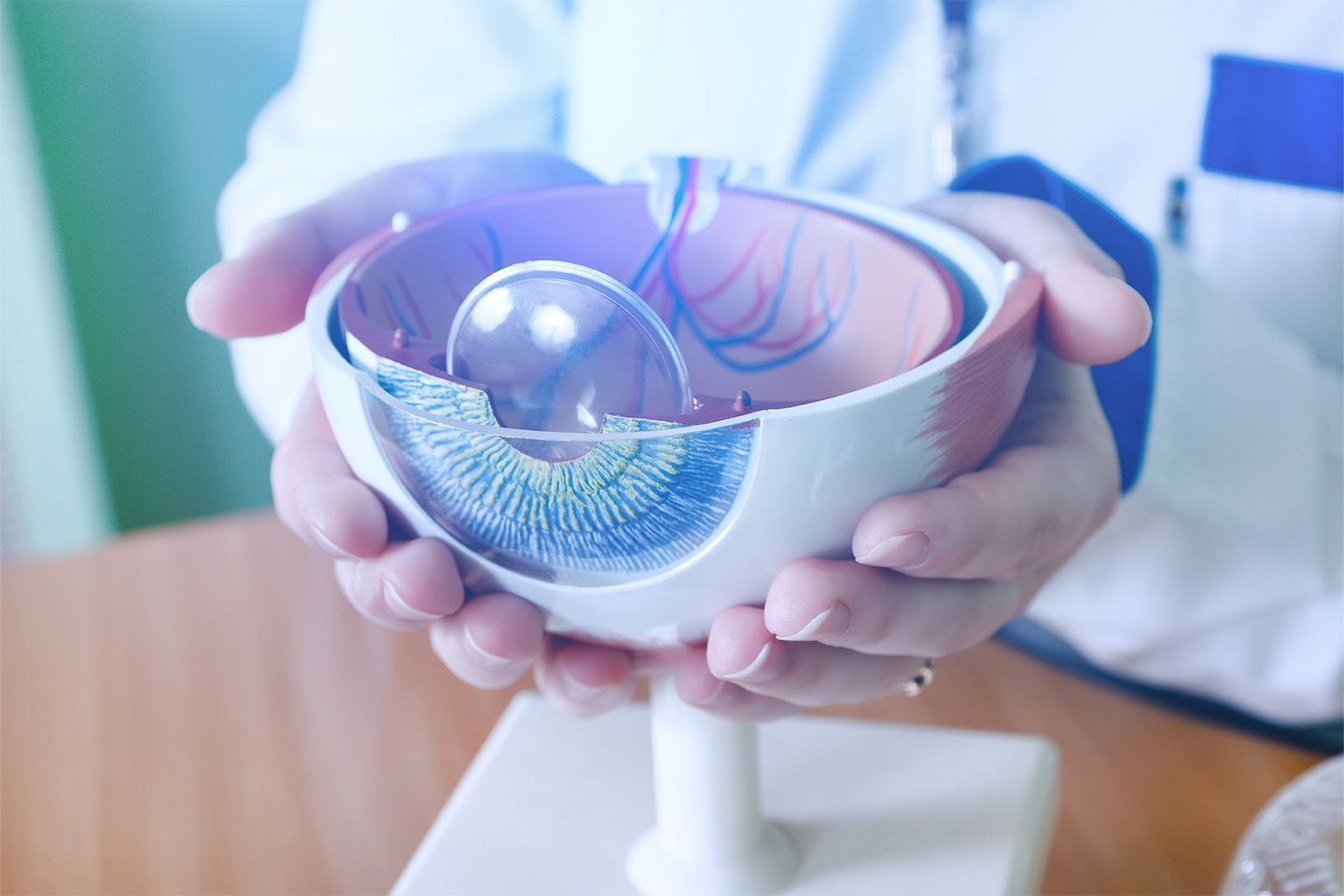
When your cornea, the front of your eye that helps focus light on the retina, can’t hold its shape properly, it may be diagnosed as keratoconus. With this condition, which usually begins in late teens and progresses for about ten years, the cornea begins to bulge, making your vision blurry or distorted. Slit lamp examination, a part of regular eye exams, can identify keratoconus as it progresses. More advanced technologies can identify it earlier and play an important role in monitoring keratoconus treatment..
Causes and Risk Factors for Keratoconus
Factors that contribute towards the development of keratoconus include excessive eye rubbing and eye allergies. It may have genetic origins for some patients, and it seems to be more common in patients with connective tissue disorders such as Marfan and Ehlers-Danlos syndromes. There are a variety of other risk factors including retinitis pigmentosa, down syndrome, sleep apnea, and a family history of keratoconus.
5 Keratoconus Symptoms
Keratoconus symptoms are typical of corneal issues and include blurry vision, seeing straight lines as wavy, and low tolerance for bright light. When you visit our ophthalmologists in Denver, mention these concerns during your regular eye exam and that will help our doctors look for cornea-related conditions such as keratoconus. Your medical and vision history provides important and diagnostically helpful clues:
- Progressively worsening vision quality beginning in early adolescence, sometimes earlier
- Frequent and unsatisfactory eyeglass prescription changes
- Contact lens changes from regular to toric (for astigmatism) to rigid gas permeable lenses
- A history of eye rubbing or eye allergies
- Sleep apnea
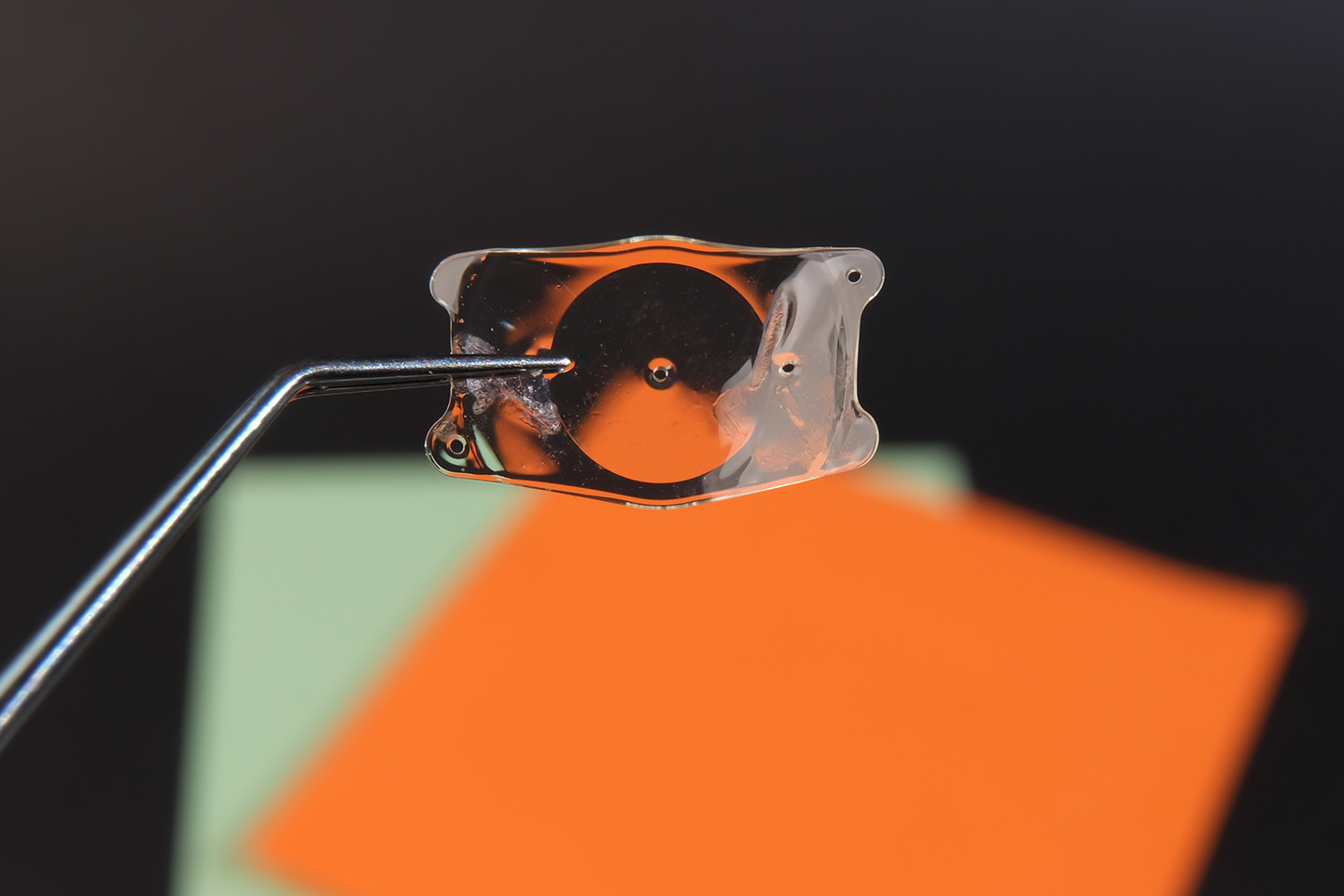
The patient’s frustrating experience of trying to find glasses or contacts that work is an important clue that can help diagnose keratoconus. Once the condition is identified, special contact lenses can be part of the solution by externally stabilizing the cornea, but that comes after a proper diagnosis of keratoconus is established.
When to See an Ophthalmologist About Possible Keratoconus
Early detection of keratoconus is important. Rapidly worsening eyesight is a sign to seek immediate eye care. Your eye doctor should be aware of any family history of keratoconus, watching carefully to see if it develops in your eyes and referring you for prompt care. Slit lamp examination, a part of regular eye exams, can identify keratoconus in very progressed stages, however, more advanced technologies can identify it much earlier. If you’re experiencing several of the symptoms listed, make an appointment with one of our eye care specialists in the Denver area who specializes in cornea care and keratoconus.
[DISPLAY_ULTIMATE_SOCIAL_ICONS]