What to Expect with Cataract Surgery: Before, During and After

From your initial consultation to the recovery process, the cataract surgery experience can seem daunting. The ICON Eyecare team has put together a comprehensive guide on what to expect before surgery, day of surgery, and in the recovery process following cataract surgery.
What is a Cataract?
![]()
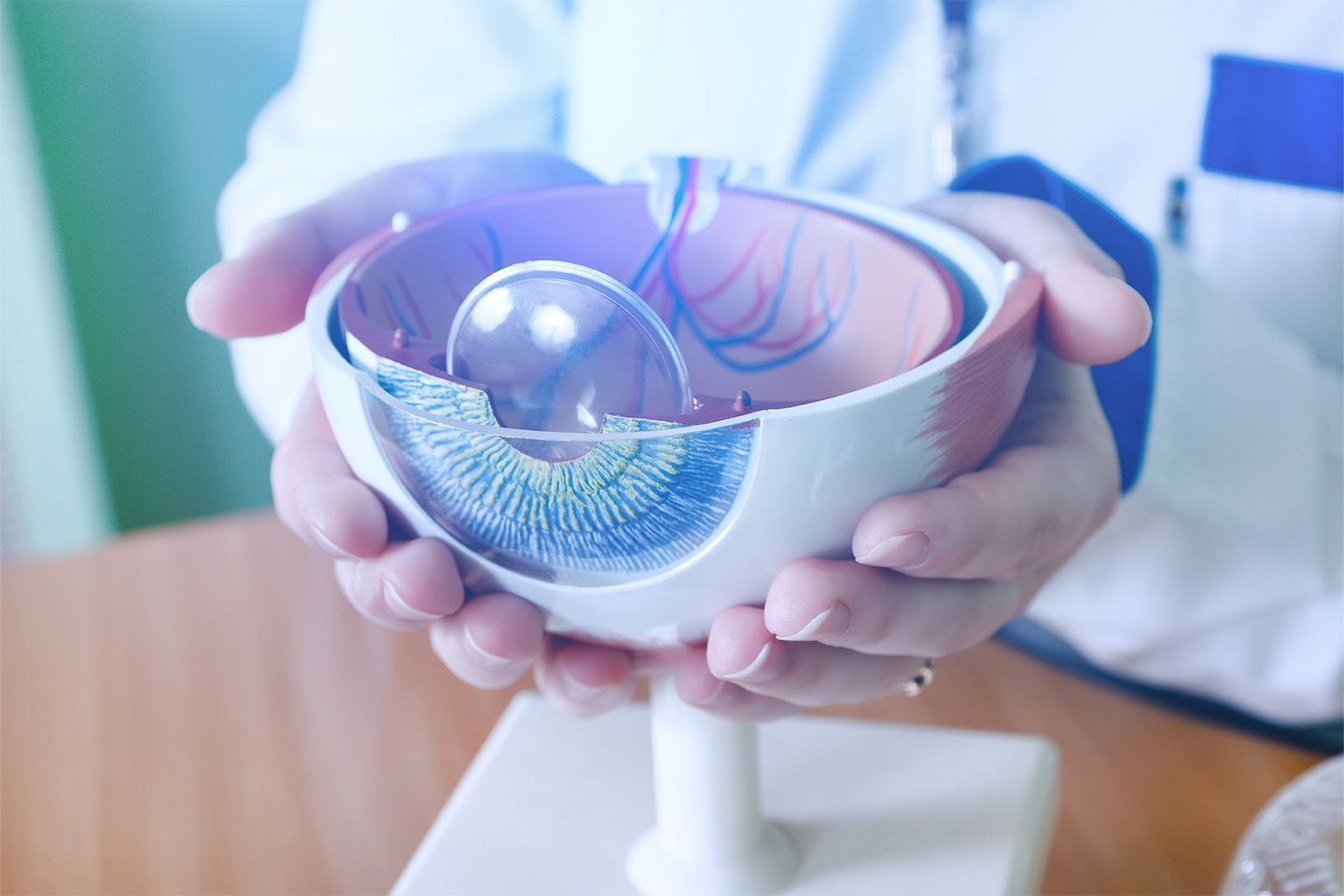
In a healthy human eye, the lens, or crystalline lens, is a clear structure that flexes to focus images onto the retina like a camera focuses an image through the lens onto film. The lens is biconvex. That means instead of one side being flat and the other being convex, both sides curve in a convex shape. A cataract is simply the body’s natural process of clouding the lens as you age. People who have cataracts experience vision changes called veiled vision, which may seem like peering through a fogged-up window.
Cataracts usually form through a slow process that gets worse with time. You can alleviate some of the earliest symptoms with brighter light and reading glasses, but eventually, cataract surgery will be required to restore clear vision.
![]()
Scheduling a Consultation for Cataracts
![]()
Patients with symptoms consistent with cataracts, or anyone with blurry vision, need to be examined by an optometrist or ophthalmologist. Many times, a diagnosis of developing cataracts requires monitoring over several years before a physician might recommend cataract surgery. Knowing that cataracts are forming is an important step in choosing preventive measures that can make the condition more comfortable. It’s important to have a baseline cataract reading with yearly monitoring by an eye doctor.
![]()
Before Cataract Surgery
It’s important that the patient discloses any medication they are taking to their eye surgeon before an invasive procedure. Some patients may be asked to halt or modify medication prior to the surgery. Your doctor may be able to provide alternative medicine that would have less effect during the preamble to surgery as well as the time involved in healing.
Patients may be asked to avoid eating or drinking for 6-8 hours before the procedure.
Some patients may need to apply eye drops before surgery.
The eye surgeon and medical team will go over every detail of the procedure and try to answer any questions the patient or their caretaker may have.
Although cataract removal surgery can be done relatively quickly in an outpatient procedure setting in your doctor’s office or surgical center, because the procedure directly affects vision, transport to and from the clinic or hospital needs to be arranged. The patient may also need help when they get home to stay comfortable and safely move around their surroundings.
During Cataract Surgery
The eye doctor will usually give the patient some medication to help them relax. Anesthetic eye drops are used to numb the patient’s eye. The surgeon will make a tiny incision to remove the affected, cloudy lens and replace it with a new intraocular replacement lens. The patient usually stays awake during this process and will be able to see general light and movement.
There is no need for stitches as the eye heals on its own in most cases. The surgeon will then apply a protective eye shield before moving the patient to the recovery room.
Types of Cataract Surgery
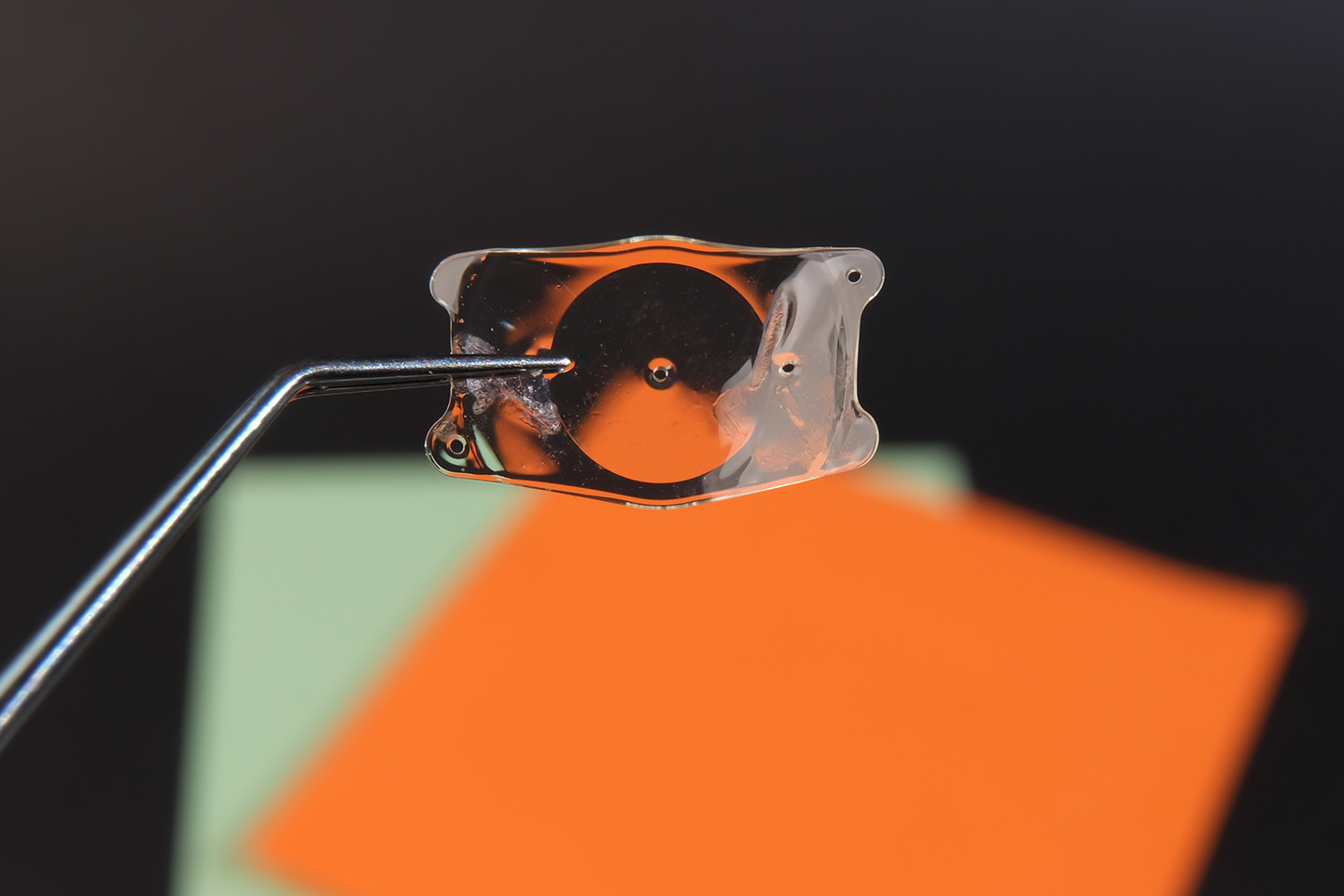
There are several types of cataract surgery designed to treat cataracts, but they all involve replacing the damaged and cloudy lens with a new one made from plastic, acrylic, or silicone.
- Small Incision Cataract Surgery (SICS) is the most common procedure performed. Your ophthalmic surgeon will make a small incision into the cornea and insert a probe that uses ultrasound waves to break up the affected lens. The small pieces can then be extracted safely, and a new, clear artificial lens called an intraocular lens (IOL) is slipped into place. This process is known as “phacoemulsification”. The surgeon will leave the original “lens capsule” in place. This is a thin natural outer membrane that normally covers the lens. Typically, the incision in the cornea does not require any sutures and is performed in an outpatient setting.
- Extracapsular Surgery involves making a larger incision in the cornea and removing the lens in one piece. The natural lens capsule is left in place, and the new lens is inserted. The surgeon may recommend this type of cataract surgery when phacoemulsification is not considered the best solution for the patient’s type of cataract. This type of surgery may require a longer recovery time.
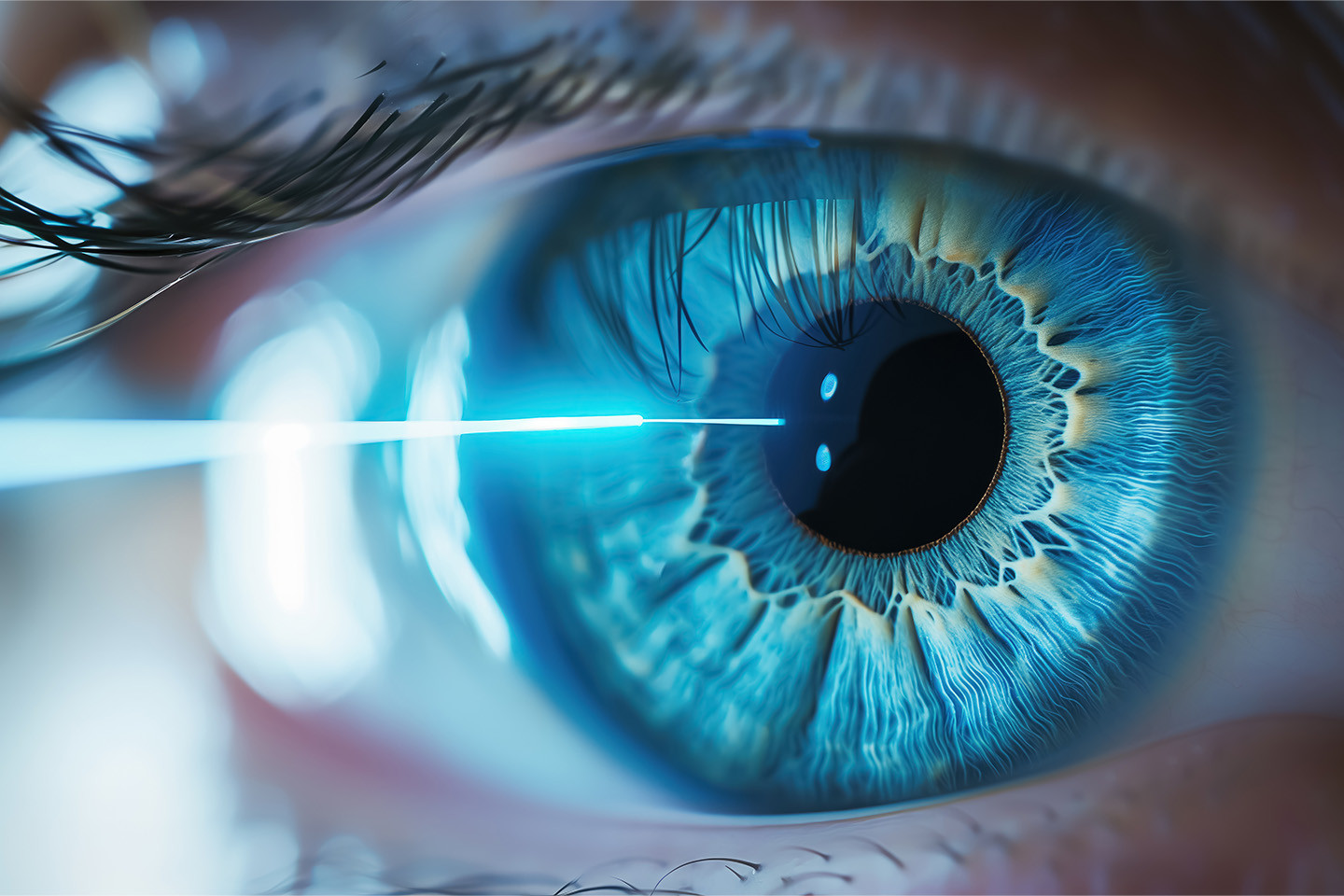
Femtosecond Laser Surgery involves a precision laser to break up the lens, whereby the surgeon removes the pieces and inserts the new lens. This can be recommended for those with astigmatism because the surgeon can reshape the cornea during the procedure for overall improved vision.
After Cataract Surgery
![]()
The patient will most likely be in the recovery room for about an hour. They will need transport home and may need a little more help than normal in the first few hours. Afterwards, they may resume much of their normal schedule, reading and watching TV while avoiding strenuous activity such as lifting anything heavy, playing sports, or jogging. Your cataract surgeon will provide you with an eye patch or eye shield to ensure protection during the healing process. They will give you instructions on when and how long you will need to wear the protective shield, and you will also receive antibacterial and anti-inflammatory eye drops that are commonly used for weeks following the surgery to help prevent infection.
It’s routine to schedule a follow-up appointment to check the affected eye the day after surgery, as well as one week later and then again after several weeks.
Cataract surgery is routinely considered a safe, painless outpatient procedure and only involves a local anesthetic. The American Society of Cataract and Refractive Surgery reports that three million Americans have cataract surgery each year with a 98-percent success rate. As with any surgical procedure, there are some cataract surgery risks. More risk is assumed by cataract patients with previous eye trauma, eye surgery, or other eye structure anomalies. If you have preexisting eye or vision problems like macular degeneration or glaucoma, your vision may take longer to recover.
When to Call Your Eye Doctor
![]()
It’s important to see an eye doctor every year. In addition to tests for vision acuity, the doctor will peer into the eye’s anatomy to assess the health of the eye and look for cataracts.
Signs and Symptoms of Cataracts
- Sensitivity to light or feeling like the light is glaring
- Noticing a “halo” around lights
- Having to strengthen your eyeglass or contact lenses for clear vision
- Experiencing double vision in one eye
- Blurred, dim, or cloudy vision
- Colors that seem to fade or “yellow”
- Needing a brighter light to read or perform tasks
- Not seeing well in the dark
When you experience cloudy or blurred vision and the eyes feel more sensitive to glare from lights, it is time to consult an eye doctor. Viewing lights in the dark that appear to have a “halo effect” is another warning sign. Increasing difficulty performing normal activities such as reading, and driving may indicate a problem. A new prescription needed for long-distance vision can be a strong indicator of cataracts forming. When these symptoms are present, you or your caregiver should schedule a consultation with your eye care professional at ICON Eyecare.
Learn More About Cataracts
Causes of Cataracts
- Aging – A person’s age can contribute to the likelihood of developing cataracts. With age, the lens will become less flexible, a little thicker, and less transparent. A cataract will scatter and/or block the light passing through to your retina, causing blurry vision and potentially vision loss.
- Traumatic Injury – Injury can contribute to developing cataracts through blunt force, a penetrating object, chemical burns, and even electric shock. It’s possible to develop cataracts years after an injury occurs.
- Medical Conditions – Some medical conditions can play a part in cataract development. Along with increasing age, some causes of cataracts may include diabetes, obesity, high blood pressure, excessive alcohol consumption, and smoking. Swelling and inflammation within the body cause cellular damage in the eye.
- Radiation Cataracts – People who spend too much time in the sun without eye protection are at risk for cataracts from UVB light, which emphasizes the importance of wearing sunglasses regularly before and after surgery.
Types of Cataracts
- Nuclear Cataracts are the most common form of cataracts and affect the center of the lens, presenting as a new nearsightedness that may actually improve your reading vision for a brief time until the lens gradually turns more yellow and clouds your vision.
- Cortical Cataracts begin with whitish streaks or spokes on the outer edge of the lens. These cataracts will eventually spread to the center of the lens and interfere with light passing through to the cornea.
- Posterior Subcapsular Cataracts affect the back of the lens. The cloudy shapes formed in the cells will diffuse the images coming through to the retina.
- Congenital Cataracts are usually present from childhood and are caused by a faulty gene from one of the parents. In almost 1 out of 5 cases, there is a history of congenital cataracts in the family history. Another cause can be intrauterine infection. Also known as chorioamnionitis, this is an infection that can affect the amniotic fluid, the umbilical cord, and the membranes surrounding the baby.
Choosing an Artificial Lens
All cataract surgeries involve the removal of the eye’s natural lens and replacing it with an artificial, clear lens called an intraocular lens (IOL). The eye surgeon will make a recommendation on which type of IOL is best based on the patient’s condition and optimal vision correction. There are several types of intraocular lenses:
- Monofocal IOLs are the most common artificial lenses and correct for a single distance. Most people set their monofocal lenses to see clearly at a distance and use reading glasses for up-close vision. Most medical insurances cover these lenses.
Other lenses listed below are considered premium options. While these lens options do provide more vision focus features, there can be some downsides, like reduced night vision, halo effects, and loss of contrast. Many find it best to correct the cataract with the common Monofocal IOLs and wear glasses for the other vision needs or vision loss.
- Multifocal IOLs are similar to bifocal or trifocal glasses. These lenses enable someone to see near and far objects, and some allow for intermediate vision, similar to progressive lenses.
- Extended depth-of-focus (EDOF) IOLs correct for one zone, usually allowing distance and intermediate vision correction.
- Accommodative Lenses correct the vision for all distances. This lens works with the natural movements of the eye’s muscles to change focus.
People with astigmatism can choose Toric Lenses with built-in correction for that condition.
Trust the Cataract Specialists at ICON Eyecare
With over 20 years of experience, ICON Eyecare’s team of board-certified cataract surgeons is committed to delivering outstanding results. As an ophthalmology practice rooted in surgical and medical services, we place the needs of our patients first and have invested in industry-leading technology, including advanced cataract lens implants and laser-assisted cataract surgery, to ensure patient safety, comfort, and high-quality results. Request an appointment today with Colorado’s cataract specialists and surgery experts.
[DISPLAY_ULTIMATE_SOCIAL_ICONS]