Laser Assisted In-Situ Keratomileusis (LASIK)

Clinical findings of LASIK
To understand LASIK it is important first to understand its development. As the name implies, “in-situ keratomileusis” was developed before Excimer laser discovery and its potential is “assisted” by the laser.
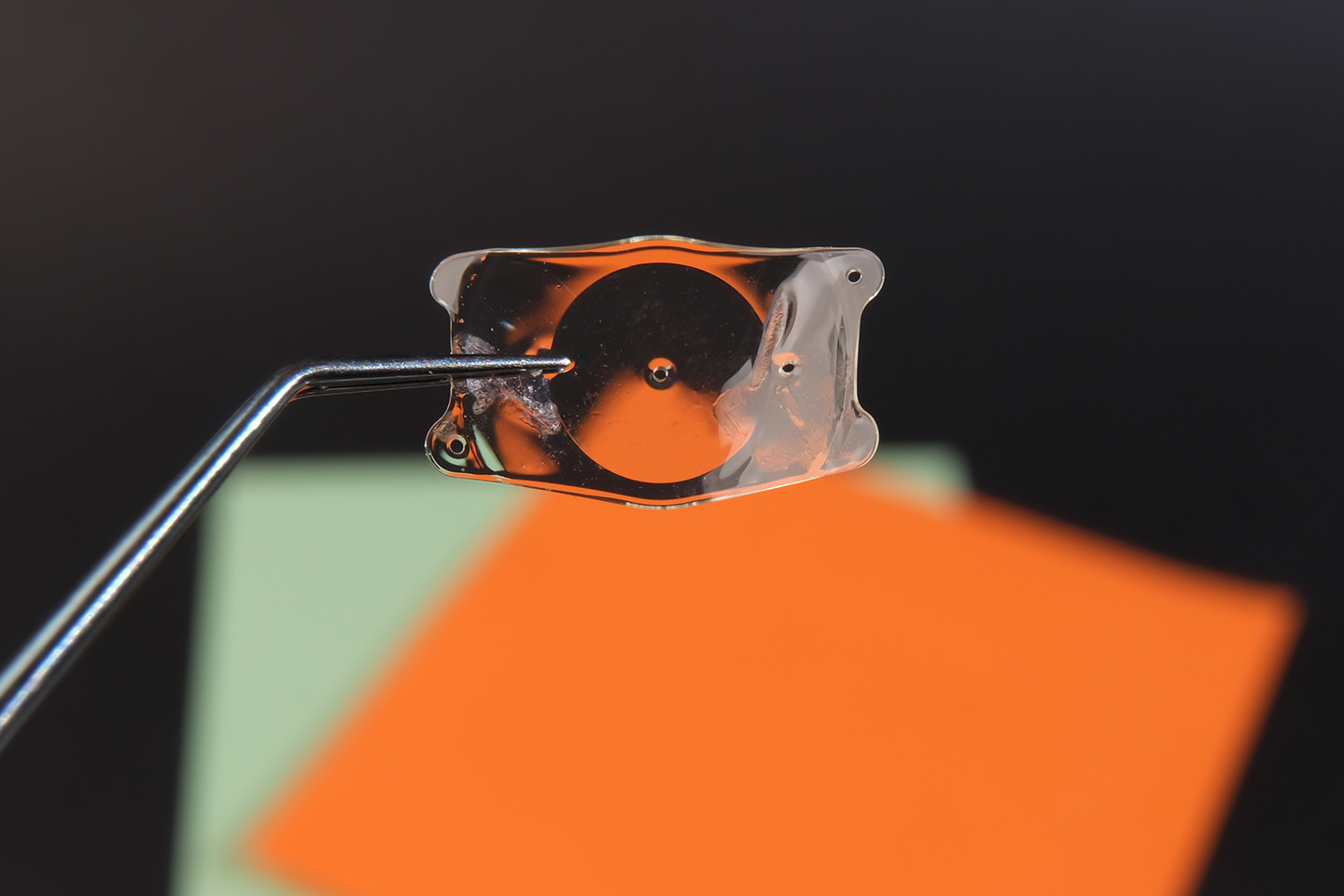
The idea then emerged to reshape the cornea by doing a refractive bisection of the remaining 2/3 of the cornea. This was done with the microkeratome performing refractive curvature change to the surface of the intact portion of the cornea. The correction required determined the depth and diameter planed off the surface of the exposed corneal stroma with the microkeratome.
The “cap” or anterior 1/3 of the cornea was then repositioned to seal and eventually heal back “in position”. Lamellar surgery dates back to 1948. Dr. Jose Barroquer originated the concept of bisecting the cornea into two sections with an instrument he termed the “microkeratome”. The anterior section of the cornea became known as the “cap” and it is approximately 1/3 of the thickness of the cornea. By 1964 the concept had advanced to a degree where human eyes were being treated to correct myopia. Initially, this consisted of using a cryolathe to reshape the freeze-dried “cap”. This further progressed to reshaping the cap without freezing it. Both methods were expensive and technically extremely challenging. The idea then emerged to reshape the cornea by doing a refractive bisection of the remaining 2/3 of the cornea. This was done with the microkeratome performing refractive curvature change to the surface of the intact portion of the cornea. The correction required determined the depth and diameter planed off the surface of the exposed corneal stroma with the microkeratome.
The flap could be lifted, turned back, and the curvature producing slice with the microkeratome could be completed and the flap turned back down. This brought procedure costs down considerably. The technical difficulty still remained.
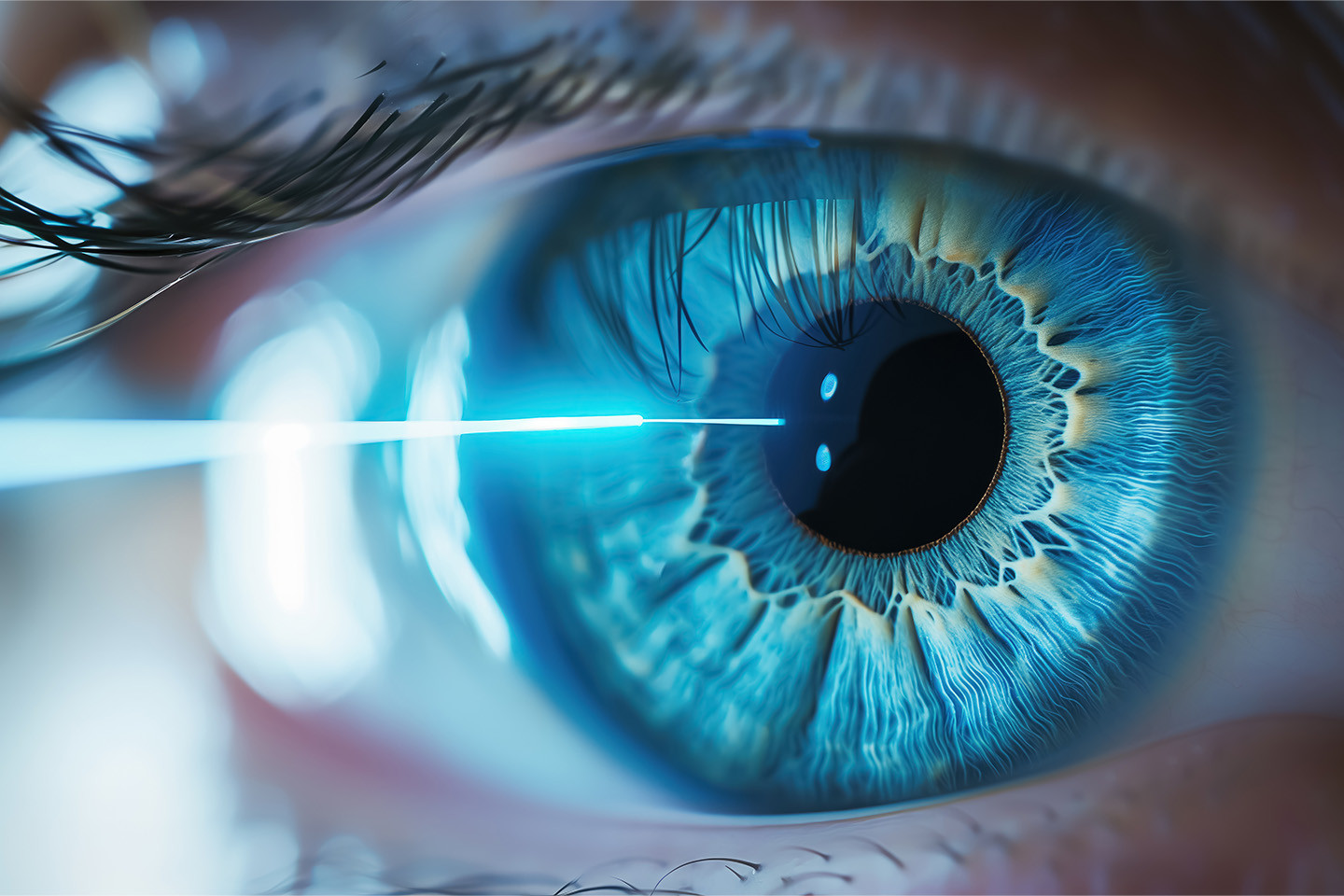
Popularity increased but complications were high and predictability nowhere near what had been with more advanced RK techniques and was now being shown with surface ablation Excimer laser. It, therefore, became a logical next move for lamellar surgeons to combine the microkeratome to form the anterior flap, approximately 1/3 of the thickness of the cornea, turn back the flap and treat the inside exposed surface with the laser. This is now known as LASIK. Top of Page When lamellar surgeons started to use the laser rather than the microkeratome to create the curvature change, they proclaimed many advantages over their present method of in-situ keratomileusis and noted advantages over photorefractive keratectomy where the epithelium was manually removed by scraping.
They noted less pain in the majority of patients. They found a faster visual recovery since the epithelium did not have to regrow (unless scratched with the microkeratome). They found a low evidence of haze formation or scarring in the interface of the two sections of the cornea.
They believed this lack of haze would allow higher myopia corrections as it was the higher myopia corrections producing the greater degree of haze with the manual method of epithelial removal. ·
They admitted that there were technical difficulties with the microkeratome but felt these could be overcome with experience and a better microkeratome.
Concerns with LASIK
Safety: Experience reduces the risk of serious vision loss due to major problems such as a penetrating cut to the eye or a partial cut scarring the visual axis, but the risks are still there. The suction produces a very high intraocular pressure which can cause optic nerve or retinal damage. These are of course are rare. Uneven cuts are not as uncommon. Irregular Astigmatism: Irregular astigmatism is the most common problem with LASIK. The data show that it occurs at about 5% or 1/20 cases. The result can be reported as 20/20 vision, but that ignores the visual quality. At present, irregular astigmatism is difficult to correct.
Healing Problems and Corneal Stability: Healing complications evolve mostly around the “cap”, a problem that is totally absent in “PRK” healing. The most common problems are: -debris left inside the cap -epithelial ingrowth under the cap -degeneration or “melting” of the cap -folds and wrinkles of Bowman’s membrane -stretching lines “striae” in Bowman’s membrane due to scarring and the cap stretching the membrane (common)
There are still many unknowns about the healing of the interface and how stable the central interface becomes. Predictability: Present data seems to indicate less accurate predictability for LASIK than for PRK. Every retreatment of the cornea adds potential complications. Suction device complications: Risks of the powerful suction device and the manually manipulated splitting of the cornea add substantial risk to the LASIK procedure.
[DISPLAY_ULTIMATE_SOCIAL_ICONS]